Stanton, B. Z., Chory, E. J. & Crabtree, G. R. Chemically induced proximity in biology and medicine. Science 359, eaao5902 (2018).
Schapira, M., Calabrese, M. F., Bullock, A. N. & Crews, C. M. Targeted protein degradation: expanding the toolbox. Nat. Rev. Drug Discov. 18, 949–963 (2019).
Schreiber, S. L. Molecular glues and bifunctional compounds: therapeutic modalities based on induced proximity. Cell Chem. Biol. 31, 1050–1063 (2024).
Yamazoe, S. et al. Heterobifunctional molecules induce dephosphorylation of kinases—a proof of concept study. J. Med. Chem. 63, 2807–2813 (2020).
Chen, P.-H. et al. Modulation of phosphoprotein activity by phosphorylation targeting chimeras (PhosTACs). ACS Chem. Biol. 16, 2808–2815 (2021).
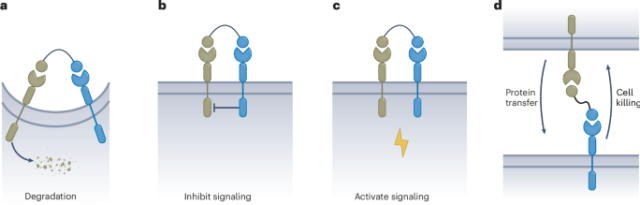
Liu, X. & Ciulli, A. Proximity-based modalities for biology and medicine. ACS Cent. Sci. 9, 1269–1284 (2023).
Gibson, W. J. et al. Bifunctional small molecules that induce nuclear localization and targeted transcriptional regulation. J. Am. Chem. Soc. 145, 26028–26037 (2023).
Ng, C. S. C., Liu, A., Cui, B. & Banik, S. M. Targeted protein relocalization via protein transport coupling. Nature 633, 941–951 (2024).
Banik, S. M. et al. Lysosome-targeting chimaeras for degradation of extracellular proteins. Nature 584, 291–297 (2020).
Cotton, A. D., Nguyen, D. P., Gramespacher, J. A., Seiple, I. B. & Wells, J. A. Development of antibody-based PROTACs for the degradation of the cell-surface immune checkpoint protein PD-L1. J. Am. Chem. Soc. 143, 593–598 (2021).
Marei, H. et al. Antibody targeting of E3 ubiquitin ligases for receptor degradation. Nature 610, 182–189 (2022).
Wells, J. A. & Kumru, K. Extracellular targeted protein degradation: an emerging modality for drug discovery. Nat. Rev. Drug Discov. 23, 126–140 (2024).
Mullard, A. First targeted protein degrader hits the clinic. Nat. Rev. Drug Discov. 18, 237–239 (2019).
Mullard, A. Targeted protein degraders crowd into the clinic. Nat. Rev. Drug Discov. 20, 247–250 (2021).
Ahn, G. et al. LYTACs that engage the asialoglycoprotein receptor for targeted protein degradation. Nat. Chem. Biol. 17, 937–946 (2021).
Pance, K. et al. Modular cytokine receptor-targeting chimeras for targeted degradation of cell surface and extracellular proteins. Nat. Biotechnol. 41, 273–281 (2023).
Ghosh, P., Dahms, N. M. & Kornfeld, S. Mannose 6-phosphate receptors: new twists in the tale. Nat. Rev. Mol. Cell Biol. 4, 202–213 (2003).
Caianiello, D. F. et al. Bifunctional small molecules that mediate the degradation of extracellular proteins. Nat. Chem. Biol. 17, 947–953 (2021).
Zhou, Y., Teng, P., Montgomery, N. T., Li, X. & Tang, W. Development of triantennary N-acetylgalactosamine conjugates as degraders for extracellular proteins. ACS Cent. Sci. 7, 499–506 (2021).
Gramespacher, J. A., Cotton, A. D., Burroughs, P. W. W., Seiple, I. B. & Wells, J. A. Roadmap for optimizing and broadening antibody-based PROTACs for degradation of cell surface proteins. ACS Chem. Biol. 17, 1259–1268 (2022).
Siepe, D. H., Picton, L. K. & Garcia, K. C. Receptor elimination by E3 ubiquitin ligase recruitment (REULR): a targeted protein degradation toolbox. ACS Synth. Biol. 12, 1081–1093 (2023).
Lau de, W., Peng, W. C., Gros, P. & Clevers, H. The R-spondin/Lgr5/Rnf43 module: regulator of Wnt signal strength. Genes Dev. 28, 305–316 (2014).
Sampathkumar, P. et al. Targeted protein degradation systems to enhance Wnt signaling. eLife 13, RP93908 (2024).
Zheng, J. et al. Bifunctional compounds as molecular degraders for integrin-facilitated targeted protein degradation. J. Am. Chem. Soc. 144, 21831–21836 (2022).
Morimoto, M., Till, N. A. & Bertozzi, C. R. Tumor immune cell targeting chimeras (TICTACs) for targeted depletion of macrophage-associated checkpoint receptors. Preprint at bioRxiv https://doi.org/10.1101/2023.12.06.570444 (2023).
Dovedi, S. J. et al. Design and efficacy of a monovalent bispecific PD-1/CTLA4 antibody that enhances CTLA4 blockade on PD-1+ activated T cells. Cancer Discov. 11, 1100–1117 (2021).
Moores, S. L. et al. A novel bispecific antibody targeting EGFR and cMet is effective against EGFR inhibitor-resistant lung tumors. Cancer Res. 76, 3942–3953 (2016).
Ludwig, S. D. et al. Multiparatopic antibodies induce targeted downregulation of programmed death-ligand 1. Cell Chem. Biol. 31, 904–919 (2024).
Chen, S., Cui, J., Chen, H., Yu, B. & Long, S. Recent progress in degradation of membrane proteins by PROTACs and alternative targeted protein degradation techniques. Eur. J. Med. Chem. 262, 115911 (2023).
Chen, X., Zhou, Y., Zhao, Y. & Tang, W. Targeted degradation of extracellular secreted and membrane proteins. Trends Pharmacol. Sci. 44, 762–775 (2023).
Ahn, G., Banik, S. M. & Bertozzi, C. R. Degradation from the outside in: targeting extracellular and membrane proteins for degradation through the endolysosomal pathway. Cell Chem. Biol. 28, 1072–1080 (2021).
Zhang, D. et al. Transferrin receptor targeting chimeras for membrane protein degradation. Nature 638, 787–795 (2025).
Sibley, D. R., Benovic, J. L., Caron, M. G. & Lefkowitz, R. J. Phosphorylation of cell surface receptors: a mechanism for regulating signal transduction pathways. Endocr. Rev. 9, 38–56 (1988).
Billadeau, D. D. & Leibson, P. J. ITAMs versus ITIMs: striking a balance during cell regulation. J. Clin. Invest. 109, 161–168 (2002).
Chakraborty, A. K. & Weiss, A. Insights into the initiation of TCR signaling. Nat. Immunol. 15, 798–807 (2014).
Monroe, J. G. ITAM-mediated tonic signalling through Pre-BCR and BCR complexes. Nat. Rev. Immunol. 6, 283–294 (2006).
Ben Mkaddem, S., Benhamou, M. & Monteiro, R. C. Understanding Fc receptor involvement in inflammatory diseases: from mechanisms to new therapeutic tools. Front. Immunol. 10, 811 (2019).
Suber, J. & Iweala, O. I. Strategies for mast cell inhibition in food allergy. Yale J. Biol. Med. 93, 719–731 (2020).
Gomez, G. Current strategies to inhibit high affinity FcεRI-mediated signaling for the treatment of allergic disease. Front. Immunol. 10, 175 (2019).
Zhu, D., Kepley, C. L., Zhang, M., Zhang, K. & Saxon, A. A novel human immunoglobulin Fcγ–Fcɛ bifunctional fusion protein inhibits FcɛRI-mediated degranulation. Nat. Med. 8, 518–521 (2002).
Daëron, M. et al. The same tyrosine-based inhibition motif, in the intracytoplasmic domain of Fc γ RIIB, regulates negatively BCR-, TCR-, and FcR-dependent cell activation. Immunity 3, 635–646 (1995).
Turner, H. & Kinet, J.-P. Signalling through the high-affinity IgE receptor FcεRI. Nature 402, 24–30 (1999).
Tam, S. W., Demissie, S., Thomas, D. & Daëron, M. A bispecific antibody against human IgE and human FcγRII that inhibits antigen-induced histamine release by human mast cells and basophils. Allergy 59, 772–780 (2004).
Zhu, D. et al. A chimeric human–cat fusion protein blocks cat-induced allergy. Nat. Med. 11, 446–449 (2005).
Eggel, A. et al. Inhibition of ongoing allergic reactions using a novel anti-IgE DARPin–Fc fusion protein. Allergy 66, 961–968 (2011).
Zellweger, F. et al. A novel bispecific DARPin targeting FcγRIIB and FcεRI-bound IgE inhibits allergic responses. Allergy 72, 1174–1183 (2017).
Veri, M.-C. et al. Therapeutic control of B cell activation via recruitment of Fcγ receptor IIb (CD32B) inhibitory function with a novel bispecific antibody scaffold. Arthritis Rheum. 62, 1933–1943 (2010).
Karnell, J. L. et al. CD19 and CD32b differentially regulate human B cell responsiveness. J. Immunol. 192, 1480–1490 (2014).
Chu, S. Y. et al. Suppression of rheumatoid arthritis B cells by XmAb5871, an anti-CD19 antibody that coengages B cell antigen receptor complex and Fcγ receptor IIb inhibitory receptor. Arthritis Rheumatol. 66, 1153–1164 (2014).
Perugino, C. A. et al. Evaluation of the safety, efficacy, and mechanism of action of obexelimab for the treatment of patients with IgG4-related disease: an open-label, single-arm, single centre, phase 2 pilot trial. Lancet Rheumatol. 5, e442–e450 (2023).
Crocker, P. R., Paulson, J. C. & Varki, A. Siglecs and their roles in the immune system. Nat. Rev. Immunol. 7, 255–266 (2007).
Paul, S. P., Taylor, L. S., Stansbury, E. K. & McVicar, D. W. Myeloid specific human CD33 is an inhibitory receptor with differential ITIM function in recruiting the phosphatases SHP-1 and SHP-2. Blood 96, 483–490 (2000).
McCord, K. A. et al. Dissecting the ability of Siglecs to antagonize Fcγ receptors. ACS Cent. Sci. 10, 315–330 (2024).
Ikehara, Y., Ikehara, S. K. & Paulson, J. C. Negative regulation of T cell receptor signaling by Siglec-7 (P70/AIRM) and Siglec-9. J. Biol. Chem. 279, 43117–43125 (2004).
Enterina, J. R., Jung, J. & Macauley, M. S. Coordinated roles for glycans in regulating the inhibitory function of CD22 on B cells. Biomed. J. 42, 218–232 (2019).
Movsisyan, L. D. & Macauley, M. S. Structural advances of Siglecs: insight into synthetic glycan ligands for immunomodulation. Org. Biomol. Chem. 18, 5784–5797 (2020).
Macauley, M. S. et al. Antigenic liposomes displaying CD22 ligands induce antigen-specific B cell apoptosis. J. Clin. Invest. 123, 3074–3083 (2013).
Duong, B. H. et al. Decoration of T-independent antigen with ligands for CD22 and Siglec-G can suppress immunity and induce B cell tolerance in vivo. J. Exp. Med. 207, 173–187 (2009).
Orgel, K. A. et al. Exploiting CD22 on antigen-specific B cells to prevent allergy to the major peanut allergen Ara h 2. J. Allergy Clin. Immunol. 139, 366–369 (2017).
Niiro, H. & Clark, E. A. Regulation of B-cell fate by antigen-receptor signals. Nat. Rev. Immunol. 2, 945–956 (2002).
Islam, M. et al. Suppressing immune responses using Siglec ligand-decorated anti-receptor antibodies. J. Am. Chem. Soc. 144, 9302–9311 (2022).
Duan, S. et al. CD33 recruitment inhibits IgE-mediated anaphylaxis and desensitizes mast cells to allergen. J. Clin. Invest. 129, 1387–1401 (2021).
Duan, S. et al. Nanoparticles displaying allergen and Siglec-8 ligands suppress IgE–FcεRI-mediated anaphylaxis and desensitize mast cells to subsequent antigen challenge. J. Immunol. 206, 2290–2300 (2021).
Fernandes, R. A. et al. Immune receptor inhibition through enforced phosphatase recruitment. Nature 586, 779–784 (2020).
Patsoukis, N., Wang, Q., Strauss, L. & Boussiotis, V. A. Revisiting the PD-1 pathway. Sci. Adv. 6, eabd2712 (2020).
Ren, J. et al. Induced CD45 proximity potentiates natural killer cell receptor antagonism. ACS Synth. Biol. 11, 3426–3439 (2022).
Finney, H. M., Rapecki, S. E., Wright, M. J. & Tyson, K. L. Molecules with specificity for CD45 and CD79. US patent US10774152B2 (2020).
Wu, S. et al. Aptamer-based enforced phosphatase-recruiting chimeras inhibit receptor tyrosine kinase signal transduction. J. Am. Chem. Soc. 146, 22445–22454 (2024).
Schmid, E. M. et al. Size-dependent protein segregation at membrane interfaces. Nat. Phys. 12, 704–711 (2016).
Waldmann, T. A. Cytokines in cancer immunotherapy. Cold Spring Harb. Perspect. Biol. 10, a028472 (2018).
Saxton, R. A., Glassman, C. R. & Garcia, K. C. Emerging principles of cytokine pharmacology and therapeutics. Nat. Rev. Drug Discov. 22, 21–37 (2023).
Liu, J. et al. Wnt/β-catenin signalling: function, biological mechanisms, and therapeutic opportunities. Signal Transduct. Target. Ther. 7, 3 (2022).
Goetz, R. & Mohammadi, M. Exploring mechanisms of FGF signalling through the lens of structural biology. Nat. Rev. Mol. Cell Biol. 14, 166–180 (2013).
Lai, Y. & Dong, C. Therapeutic antibodies that target inflammatory cytokines in autoimmune diseases. Int. Immunol. 28, 181–188 (2016).
Kim, G. W. et al. IL-6 inhibitors for treatment of rheumatoid arthritis: past, present, and future. Arch. Pharm. Res. 38, 575–584 (2015).
Hernandez, R., Põder, J., LaPorte, K. M. & Malek, T. R. Engineering IL-2 for immunotherapy of autoimmunity and cancer. Nat. Rev. Immunol. 22, 614–628 (2022).
Junttila, I. S. et al. Redirecting cell-type specific cytokine responses with engineered interleukin-4 superkines. Nat. Chem. Biol. 8, 990–998 (2012).
Harris, K. E. et al. A bispecific antibody agonist of the IL-2 heterodimeric receptor preferentially promotes in vivo expansion of CD8 and NK cells. Sci. Rep. 11, 10592 (2021).
Yen, M. et al. Facile discovery of surrogate cytokine agonists. Cell 185, 1414–1430 (2022).
Romei, M. G. et al. i-shaped antibody engineering enables conformational tuning of biotherapeutic receptor agonists. Nat. Commun. 15, 642 (2024).
Sonoda, J., Chen, M. Z. & Baruch, A. FGF21-receptor agonists: an emerging therapeutic class for obesity-related diseases. Horm. Mol. Biol. Clin. Investig. 30, 20170002 (2017).
Geng, L., Lam, K. S. L. & Xu, A. The therapeutic potential of FGF21 in metabolic diseases: from bench to clinic. Nat. Rev. Endocrinol. 16, 654–667 (2020).
Fon Tacer, K. et al. Research resource: comprehensive expression atlas of the fibroblast growth factor system in adult mouse. Mol. Endocrinol. 24, 2050–2064 (2010).
Xie, Y. et al. FGF/FGFR signaling in health and disease. Signal Transduct. Target. Ther. 5, 181 (2020).
Véniant, M. M. et al. Long-acting FGF21 has enhanced efficacy in diet-induced obese mice and in obese rhesus monkeys. Endocrinology 153, 4192–4203 (2012).
Smith, R. et al. FGF21 can be mimicked in vitro and in vivo by a novel anti-FGFR1c/β-klotho bispecific protein. PLoS ONE 8, e61432 (2013).
Kolumam, G. et al. Sustained brown fat stimulation and insulin sensitization by a humanized bispecific antibody agonist for fibroblast growth factor receptor 1/βklotho complex. eBioMedicine 2, 730–743 (2015).
Ming, A. Y. K. et al. Dynamics and distribution of klothoβ (KLB) and fibroblast growth factor receptor-1 (FGFR1) in living cells reveal the fibroblast growth factor-21 (FGF21)-induced receptor complex. J. Biol. Chem. 287, 19997–20006 (2012).
Wong, C. et al. Fibroblast growth factor receptor 1/klothoβ agonist BFKB8488A improves lipids and liver health markers in patients with diabetes or NAFLD: a phase 1b randomized trial. Hepatology 78, 847–862 (2023).
Gordon, M. D. & Nusse, R. Wnt signaling: multiple pathways, multiple receptors, and multiple transcription factors. J. Biol. Chem. 281, 22429–22433 (2006).
Clevers, H., Loh, K. M. & Nusse, R. An integral program for tissue renewal and regeneration: Wnt signaling and stem cell control. Science 346, 1248012 (2014).
Post, Y. et al. Design principles and therapeutic applications of novel synthetic WNT signaling agonists. iScience 27, 109938 (2024).
Janda, C. Y. et al. Surrogate Wnt agonists that phenocopy canonical Wnt and β-catenin signalling. Nature 545, 234–237 (2017).
Tao, Y. et al. Tailored tetravalent antibodies potently and specifically activate Wnt/Frizzled pathways in cells, organoids and mice. eLife 8, e46134 (2019).
Miao, Y. et al. Next-generation surrogate Wnts support organoid growth and deconvolute Frizzled pleiotropy in vivo. Cell Stem Cell 27, 840–851 (2020).
Chen, H. et al. Development of potent, selective surrogate WNT molecules and their application in defining Frizzled requirements. Cell Chem. Biol. 27, 598–609 (2020).
Hauser, A. S., Attwood, M. M., Rask-Andersen, M., Schiöth, H. B. & Gloriam, D. E. Trends in GPCR drug discovery: new agents, targets and indications. Nat. Rev. Drug Discov. 16, 829–842 (2017).
Rankovic, Z., Brust, T. F. & Bohn, L. M. Biased agonism: an emerging paradigm in GPCR drug discovery. Bioorg. Med. Chem. Lett. 26, 241–250 (2016).
Sachdev, S., Creemer, B. A., Gardella, T. J. & Cheloha, R. W. Highly biased agonism for GPCR ligands via nanobody tethering. Nat. Commun. 15, 4687 (2024).
Cheloha, R. W., Gellman, S. H., Vilardaga, J.-P. & Gardella, T. J. PTH receptor-1 signalling—mechanistic insights and therapeutic prospects. Nat. Rev. Endocrinol. 11, 712–724 (2015).
Goebeler, M.-E. & Bargou, R. C. T cell-engaging therapies — BiTEs and beyond. Nat. Rev. Clin. Oncol. 17, 418–434 (2020).
You, G. et al. Bispecific antibodies: a smart arsenal for cancer immunotherapies. Vaccines 9, 724 (2021).
Huehls, A. M., Coupet, T. A. & Sentman, C. L. Bispecific T-cell engagers for cancer immunotherapy. Immunol. Cell Biol. 93, 290–296 (2015).
Zhao, S. et al. Gnawing between cells and cells in the immune system: friend or foe? A review of trogocytosis. Front. Immunol. 13, 791006 (2022).
Li, K.-J. et al. Trogocytosis between non-immune cells for cell clearance, and among immune-related cells for modulating immune responses and autoimmunity. Int. J. Mol. Sci. 22, 2236 (2021).
Joly, E. & Hudrisier, D. What is trogocytosis and what is its purpose? Nat. Immunol. 4, 815 (2003).
Till, N., Ramanathan, M., Loh, K. Y. & Bertozzi, C. Trogocytosis targeting chimeras (TrogoTACs) for targeted protein transfer. Preprint at ChemRxiv https://doi.org/10.26434/chemrxiv-2024-k7kn2-v2 (2024).